Having a baby is a pretty overwhelming experience, even if all goes smoothly. No matter the amount of research you’ve done, books you’ve read, baby items you’ve bought, parenting podcasts you’ve listened to, when you take that baby home with you for the first time, you find yourself staring at it blankly, trying to remember what to do. But if you’re like me and you had a baby that was admitted to the neonatal intensive care unit, having a baby doesn’t just feel overwhelming, it can be downright traumatic.
There is no conclusive reason for why I went into early labour – it is assumed that it was brought on by a UTI as my infection markers were elevated. But whatever the reason, my beautiful daughter, Noah Eva Heron, was born on 25th June 2020 at 02:30am. She was 12 weeks premature and weighed just 2lb 9oz.
Day One
About 15 hours after Noah was born, we finally got the go ahead to see our baby girl. I felt an overwhelming feeling of relief and fear at the same time, desperate to see her, but terrified of what I would find when I did.
Seeing Noah in the neonatal unit for the first time is a moment I will never, ever forget. My husband and I looked through the thick plastic walls of the incubator to see our daughter and tears of both joy and sadness rolled down my face. I felt relief – relief that despite everything, here she was in front of me, alive. I could see her moving and, despite how tiny she was, she was perfectly formed. I was relieved that she looked like a baby (I wasn’t sure she would) even if she was a very small, skinny one.
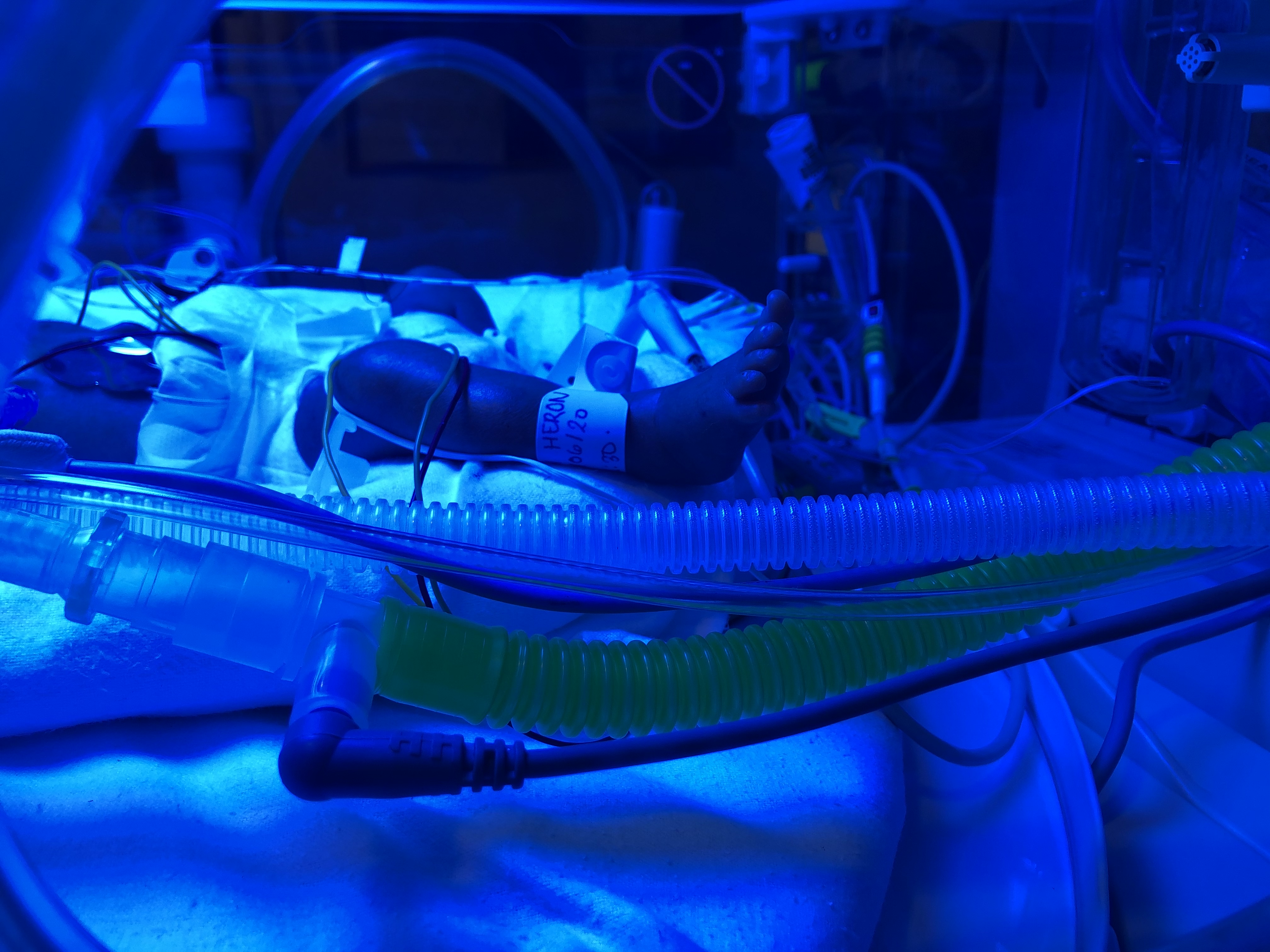
But I was also overwhelmed. This was my first time in a NICU (neonatal intensive care unit) and it was daunting. It was full of busy medical staff, incubators, beeping machines and an unsettling atmosphere of urgency. I was overwhelmed by the wires and tubes that covered her, none of which I understood at the time. She was so tiny and fragile; I could see all of her ribs as her chest rose and fell with the breaths from the ventilator. My husband had his arm around me, and I just wept as the reality of the situation started to sink in.
My brain couldn’t compute that this was my baby, the tiny baby I had been carrying for six months, who I had only just started to feel moving and kicking inside me. As I looked at her, she could have been anyone’s baby.

The nurse looking after Noah encouraged us to put our hands through the small incubator portholes to touch her. I was both desperate and terrified to touch her, scared that I might hurt her. I washed my hands meticulously and reached inside, putting my finger into her tiny palm. I tried not to think about her future, her chances, her outlook, and did my best to just enjoy our moment together. For now, this would have to be enough.
For the next three days, I stayed in the hospital as I recovered physically from the trauma of Noah’s birth. Due to giving birth with no assistance, I had a second-degree tear and needed stitches. I also had a slight infection and so was kept in for observation. This was both an advantage, as I was able to see Noah whenever I wanted, day or night, but it also had its disadvantages.
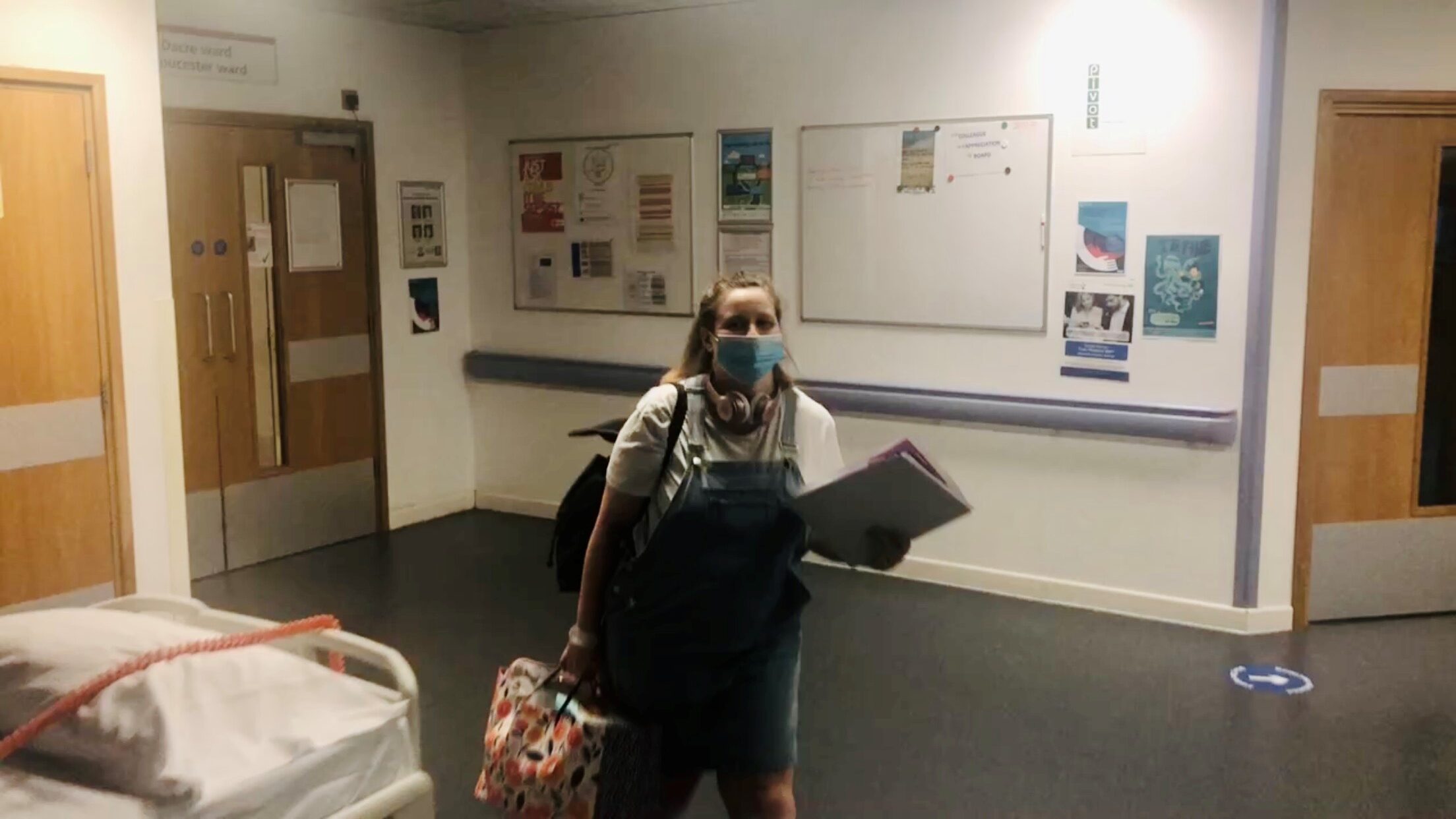
I was on a ward full of women who had just given birth, surrounded by mums wheeling their healthy babies around the corridors in their cots. The hospital staff were kind enough to put me in my own room, but at night I could still hear the cries of the newborns in the rooms next door. Hearing those cries felt like torture as I knew it was the sign of a strong and healthy baby, yet my baby was what felt like miles away in the NICU, fighting for her life. And to top it all off, as it was COVID, I wasn’t able to have any visitors, including my husband.
Day Two
Due to COVID restrictions, my husband (Jason) and I were no longer able to visit the NICU together; in fact only one parent was able to visit the ward per day. So today, I visited Noah alone.
Each morning, the doctors conducted ward rounds and I was able to sit with one of Noah’s doctors and learn more about her care. She explained that Noah was doing as well as could be expected (I was too scared to ask what that meant) and a general overview of what each of the bits of equipment were doing.

To be honest though, I didn’t take much of it in at the time, my brain was just so full of worry for my little baby. The doctor just kept asking me if there was anything else I wanted to know, but my mind kept drawing a blank – it’s hard to know what the right questions to ask are, when the only one you really want an answer to – ‘is my baby going to be ok’ – is the one they can’t answer.
The noise, alarms, terminology and general hustle and bustle of the neonatal ward is pretty overwhelming, not to mention seeing such a tiny baby connected to so many machines – my heart pretty much leapt out of my chest every time one of Noah’s alarms went off, fearing the worst. But over the next few weeks, I began to understand what each machine was doing to support her and give her the best chance of survival, and know the various things in place to alert the team when something was wrong. I wish I’d spent more time on that second day asking what each wire was for, what each machine monitored and alarm meant, as it would have been hugely reassuring – but hindsight is a wonderful thing.
- Incubator. Premature babies are usually cared for in an incubator, where their temperature is controlled and they can receive what they need safely in a stable environment. There were small holes at the sides to allow doctors, nurses and us, to touch and handle Noah. The incubator kept her warm, as premature babies can’t control their own temperature well, by feeding hot humid air in. Premature babies have very delicate skin and can lose a lot of water, so the humidity helps protect it. The incubator also kept Noah safe from the noise in the NICU, infections and all unnecessary contact.
- Phototherapy. Blue light is used for the treatment of neonatal jaundice, which is where the skin and whites of a babies eyes become yellow because of too much bilirubin in the blood. Noah was under special blue light to reduce the level of bilirubin and she wore a mask over her eyes to protect them because it was so bright.
- Cardiorespiratory monitor. Wires attached to sticky patches on Noah’s chest and tummy monitored her heart and breathing rates and showed them on a screen. Alarms would go off each time the rates dropped below what was considered ‘normal’ and every time, I would hold my breath to see if they would stabilise.
- Temperature probe. A temperature probe was put on Noah’s skin. A wire connected the temperature probe to the incubator to help regulate the heat needed to keep her warm.
Pulse oximeter. The tiny red light attached to Noah’s foot (or sometimes hand) measured the amount of oxygen in her blood through the skin. A wire connected the light to the monitor where it displayed the oxygen saturation (O2), the amount of haemoglobin in her red blood cells saturated with oxygen.
Umbilical catheter. Most babies in the NICU have an intravenous catheter (a thin, flexible tube) for giving them fluids, nutrients and medications, instead of injecting Noah every few hours. Noah’s stomach was so tiny that she wasn’t able to take all her nutrition from the milk fed to her through her NG tube, and so fluids were required to help her get all she needed to grow.
Positive pressure ventilator. Air was blown gently into Noah’s lungs through a tube which is passed through her mouth. This inflated Noah’s lungs at regular intervals, and could be adjusted depending on what she needed at the time. It is also gave her some extra oxygen as her lungs were not developed enough to get it on her own.
Scales. The scales may not be the most modern equipment in the NICU, but they are one of the most important. Milk volumes, IV liquids and medication were calculated based on the Noah’s weight and so it’s vital that the weight is accurate. Newborn babies often loose weight at first and premature babies are no different. But as they are so small in the first place, it is essential that this is limited as much as possible. Noah was weighed every day at the same to make sure everything was ok.

Today Noah came off her ventilator
Today, Noah’s ventilator got blocked and she stopped breathing. The ventilator was urgently removed, and alternative breathing support was given. When a baby is known to be arriving prematurely, mothers are usually given steroids to help mature the baby’s lungs for breathing, and magnesium sulphate for brain development. Unfortunately, due to Noah’s surprise appearance, I didn’t receive either of these treatments.
This, plus the fact that Noah wasn’t breathing when she was born, meant it was a miracle that today, Noah was successfully moved to CPAP (continuous positive airway pressure) – a non-invasive breathing support. This passes air through a small mask over her nose, raising the pressure to help keep her lungs inflated. I thank God that I wasn’t there when it happened though – I don’t think I could have handled being rushed out as they once more fought to get Noah breathing.
In spite of not being there at the time, it was still a pretty tough day to be honest. After the adrenaline of giving birth had worn off, the overwhelming relief that she was alive was overshadowed by the fear of what was to come. Although Jason wasn’t allowed onto the ward, he met me at the hospital entrance to give me a cuddle while I cried – it’s difficult enough to see your baby in intensive care, without the additional stress of having to do it on your own.
Day Three
Daddy visited Noah today and, although I was still on the ward upstairs, I couldn’t go and see my baby for the whole day due to the COVID restrictions. We like to think of it as their first daddy-daughter day of many (even if it wasn’t how either of us pictured it). Each day that we visited, we would keep the other up to date with plenty of photos and videos. Thank goodness for technology!!
Today we saw her without the blue light on for the first time – it made the bruises all over her body so much easier to see and the trauma of what she went through so much more real somehow.

It also became very noticeable how skinny she was – her skin looked so wrinkly and loose because she didn’t have much fat underneath it (this builds up in the womb during later weeks of pregnancy).
We were taught that touch is the first of a preemie’s senses to mature, and it’s through touch that Noah would initially learn about the world. Touch was also a key way for us to bond with and soothe her by placing our hands gently on her tummy and head. But we had to keep them still. Too much pressure or the wrong kind of touch can be overwhelming and stressful for a premature baby.
Another thing that was bizarre was how hairy she was all over her body. This hair is called lanugo (womb hair) and is very thin, soft hair that is normally shed before birth, around seven or eight months of gestation. It will eventually disappear on its own but it was a bit of a shock to see it all over her – on her face, arms, back, chest – literally everywhere!
I began expressing with an electric pump today. I had been encouraged to practice hand expressing up until now and it was a lot of hard work for very little reward. I always planned to exclusively breastfeed, but as Noah arrived so early, this wasn’t possible, so as far as I was concerned, expressing was the next best thing.
I began by hand expressing colostrum and it was really laborious – the first time I literally sat for 45 minutes to end up with only 0.1ml of colostrum collected. But I was assured by the nurses that every bit of colostrum was like liquid gold, packed with nutrition tailored to Noah. So I persisted, religiously expressing every three hours in the day, every four at night. The electric pump was a game changer. The first time, I collected 20ml within 20 minutes. I felt like an absolute boss-mum.

Day Four
Today was a very difficult day. They tried inserting a new line for Noah’s fluids called a long line – a fine plastic tube that was threaded into one of the small veins from her foot, along her leg to just outside the heart. Her fluids can then be given through this line and, because it emerges into a larger vein, the risk of damage to her veins is much lower. The umbilical catheter was the most efficient way to deliver fluids, but is only temporary. Once in place, the long line can stay in place for several weeks, if necessary, which reduces the number of times Noah will need to have a drip inserted.

Once the long line is inserted, an x-ray is used to check whether it is in place. However, because of how small she is, they were unable to position the line correctly, despite two further attempts to re-position. The decision was made to take it out and try again another day. It was devastating. Each time the line was inserted or readjusted it was extremely distressing for Noah and it broke my heart to see her going through so much. That’s the thing with premature or very poorly babies – they have been through in their short little lives more medical procedures than most will experience in their lifetime.
But Noah is doing better. She was taken off the blue light today as her bilirubin is at a level where she should be able to manage it herself. Every parent celebrates milestones that their babies reach – smiling, giggling, rolling over, sitting up, walking – preemie babies just have an extra set of milestones that they work through, meaning more reasons for us as their parents to celebrate.

Today Noah no longer needed light therapy
I was discharged from hospital today. It was bitter-sweet as I was finally able to go home to my husband and my bed, but it meant I had to leave my beautiful baby girl in hospital. I felt so guilty for leaving her and sobbed in the hospital car park. It’s really hard to leave your baby in the hospital and head home for the first time. When I had dreamed about having Noah, something that I took for granted was that when she was born, we would be her primary carers. But the reality is that Noah needed much more support than I was able to give – for the first 8 weeks of her life, I had to leave that to her doctors and nurses, and that hit me harder than I thought it would.
Day Five
In that first week, I remember finding it almost impossible to look ahead, to even contemplate the next day, let alone any further. Whenever I did, my anxiety would spiral as the only future I could see clearly was one where I wouldn’t be bringing Noah home. It was only possible to make it through each day by being in the moment, focussing on the now, and leaving tomorrow up to God to determine.
But each day, each step of progress Noah made, no matter how tiny, brought a different future more and more into focus – a possibility of bringing my beautiful baby girl home, happy and healthy. Today they managed to insert the new feeding line and remove the umbilical catheter all together, a step that felt monumental.
Noah was also due to have more routine blood tests today. These are among the most frequent procedures in the NICU and they provide crucial information on how she is doing, or alert doctors if something is wrong before it causes further problems. They are able to check for iron (anemia), bilirubin (jaundice), blood sugar (hypoglycemia), a salt or water imbalance, nutritional needs (such as problems with protein or liver and kidney function), infection markers and blood gases (oxygen and carbon dioxide). These can all cause problems if not fixed early.

It’s incredibly difficult for the doctors to locate and enter a premature baby’s teeny-tiny veins – all sorts of things can go wrong. No matter how many times you see your baby have these routine blood tests, it never gets any easier. Today was really hard to watch as they struggled to take her blood. Noah was getting more and more distressed – it was so difficult to stand by and watch as she cried and cried and, despite knowing how essential they are, I wanted to jump in and stop the doctors from hurting my precious little girl. Unfortunately they just couldn’t get the blood they needed so they had to stop and try again later in the day. The second time they came to take the bloods they were successful – thank the Lord!

Today Noah’s umbilical catheter was removed
However, despite the high of removing the umbilical line in the morning, we were brought back down to earth with a bump as there were further issues with the long line that evening. This meant it had to be readjusted for the third time – another uncomfortable procedure for our unbelievably resilient baby girl.
Day Six
Today we were allowed to put toys in Noah’s incubator. This was the first time that we were able to give something to our baby, which may not seem like much, but to us it felt like such a momentous step.
Before Noah was born, we had (like so many other parents when getting ready for a new arrival) been dreaming of the day we could bring her home from the hospital, what clothes we would dress her in, the moses basket she would sleep in, and the tiny teddies we would buy for her to snuggle up with. But her story up until now was far from the way we pictured it. This small gift felt like us claiming back a part of that dream that had been stolen as we were finally able to give our little girl a part of what we had planned for her.

Today Noah came of CPAP and we were able to give her first gift
Noah was getting stronger each day. The CPAP was removed and we were finally able to see her whole face! It was incredible! But she still needed some oxygen and a constant flow of air into her lungs to keep her premature lungs properly inflated through a nasal cannular. By now, she was taking all of her own breaths, but the constant pressure was there to ‘remind’ her to breathe.
I was hoping to finally be able to hold her today, but once again they had some trouble with the long line. Again, they had to carry out the procedure to attempt to reposition the line as it had moved a little high in her artery. This can be really distressing for such tiny babies and Noah needed to rest and be moved as little as possible.

Day Seven
Today was a good day! Finally I got to hold my baby for the first time. It was such a mixture of emotions. Although I was so overjoyed that I was finally holding my daughter, it was also different to how I imagined. Rather than the love and excitement I was expecting to feel, I felt incredibly nervous and strangely distant from the fragile baby I held in my arms – out of her incubator she looked even stranger and more alien like than I was expecting. I felt so blessed she was here, but also heartbroken all over again about the fight she was having to face. And I had to experience it alone because of COVID. I just looked at her while desperately praying, worshipping and crying for the whole hour.
Jason also went to register her birth today, so she officially became ‘Noah Eva Heron’. This was something that I was unsure of doing at first – it sounds awful but I was scared of making her ‘official’ in case she passed away. Did it make her more real somehow? Would that make it harder if the time came to say goodbye? Ultimately though, like with announcing her birth on social media, we made the decision that she was absolutely alive and real, and that she deserved to be recognised and celebrated.


Today we were able to have our first cuddles
It such a weird one when you have a premature baby. Noone quite knows what to say, or whether to congratulate you. I didn’t entirely know the right way to feel myself to be honest (not that there is a right way, I know that now).
It is a difficult one, I admit. But a baby has just been born – that’s a miracle! The circumstances may be unexpected and far from ideal, and it may not be a celebratory experience, but we felt it was still so important to recognise her birth. And the congratulatory messages we received really helped us to celebrate the little miracle in front of us, even when we weren’t sure how long we would get to enjoy her for.
Noah also began to open her eyes today (although it was a lot of effort so they were barely open for a second before they closed again). She also had a black eye beginning to show, due to the trauma she experienced at her birth, which probably didn’t help. I just remember thinking they were so big, dark and how incredibly beautiful she was!
I also remember being incredibly emotional as she looked at me for the first time, wondering if she recognised me as her mum from the six months I’d been carrying her around. But again, with everything in the NICU, I also felt so incredibly sad as the realisation hit that the first faces she’d seen were of the hospital staff, not her mummy or daddy, and that she wouldn’t see a face without a mask for another couple of months.


Today I changed Noah’s nappy for the first time
Another first though – I got to change Noah’s nappy for the first time, with lots of help from the NICU nurse when navigating the wires. When finding out I was pregnant, I’m going to be honest, one of the things that I was most apprehensive about was the nappy changes – would I cope with how disgusting babies nappies were? But in that moment I was so excited to just be able to do something as normal as change her nappy (she was kind to me and made sure it was only a wet one for my first time).
Overall though, I remember leaving the hospital feeling really happy for the first time that day. I’d cuddled, changed and looked into my baby’s eyes for the first time, and the doctors had reassured me that they were really pleased and ‘proud’ of her progress.
That first week, the fear of losing Noah was immense and all-consuming. Our lives had been turned upside down, we had so much new medical information to digest and a complicated new routine to accept. But the positive thing was that, one week in, I was finally starting to experience some of that unconditional, motherly love that everyone was talking about. Some. We still had a long way to go.

Leave a Reply